Principles of Paediatric Extremity Trauma in the Deployed Setting
What's new / Latest updates
This is the first iteration of this guideline
Objectives
The objective of this CGO is to outline the identification, assessment, and management of paediatric extremity trauma in the deployed setting. This CGO is not exhaustive in its own right, but is meant to highlight the main considerations in the paediatric population that differ from those in adults. It should be read and understood as an adjunct to UK TCCC teaching.
Scope
This guideline is intended to provide basic guidance for immediate management of paediatric extremity trauma within the deployed surgical care setting (Role 2 and Role 3).
Audience
The target audience is deployed surgical teams.
Initial Assessment & Management
Initial assessment should be according to UK TCCC and includes a systematic assessment / management of:
M - Massive Haemorrhage
A - Airway
R - Respiratory system
C - Circulation
H - Hypothermia mitigation/ head injury
Link to Page per Age for Physiological Parameters and Drug Dosages
Advanced Assessment & Management
Massive Haemorrhage
Uncontrolled massive haemorrhage must be controlled immediately. Initial management should be with direct pressure, application of a CAT (Combat Application Tourniquet). In adults, tourniquet times are generally recommended between 2-4 hours with reduced limb salvage and higher mortality over 4 hours. There is no specific information related to paediatric tourniquet times but keeping ischaemic time as short as possible is advised as per the adult guidance.
A range of additional measures may be required to control extremity haemorrhage including: direct or indirect pressure, compression bandaging, and topical haemostatic agents.
Patients arriving at your echelon of care with a tourniquet in situ should be re-assessed at the earliest opportunity to determine if it is still required.
Link to CGO on Control of Major Haemorrhage
Limb Salvage and Neurovascular Assessment
Neurological and vascular status of the limb should be assessed and recorded distal to the injury. Every effort must be made to record these findings at the initial presentation:
- Temperature
- Pulses (including doppler if available)
- Capillary Refill Time
- Sensation and Movement
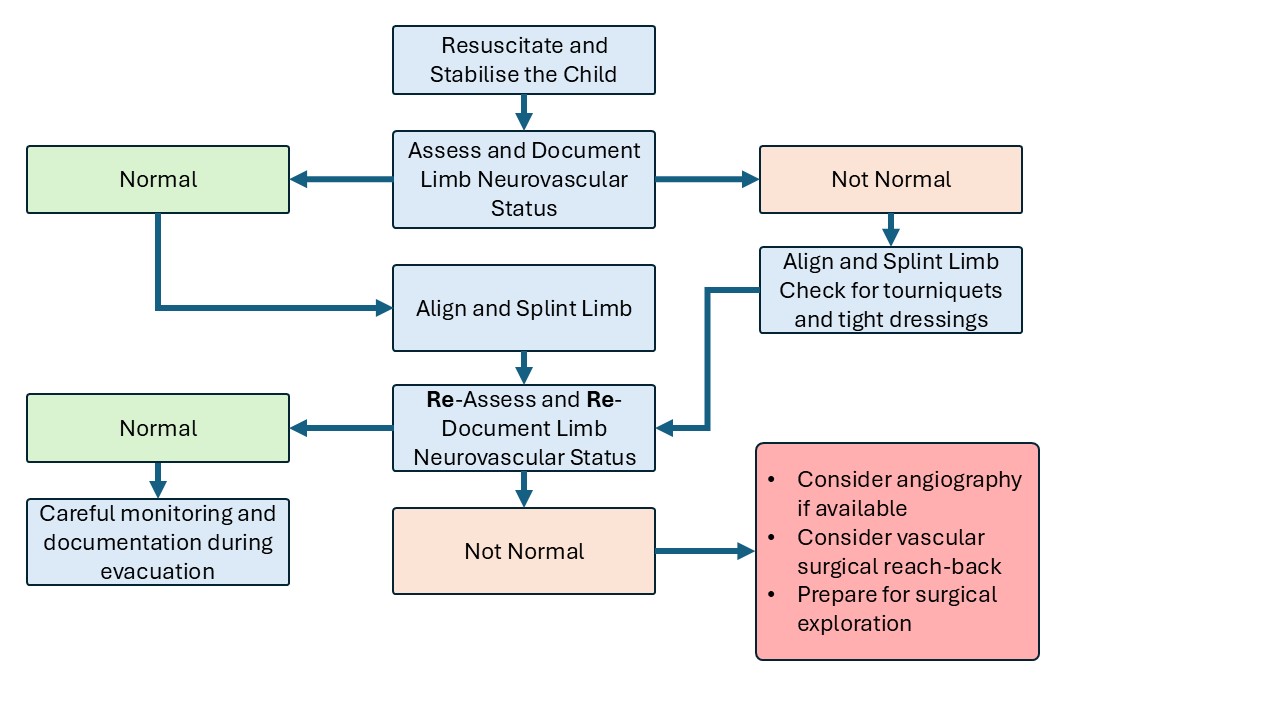
If there are concerns regarding perfusion distal to the injury the initial management should be anatomical alignment of the limb and splinting. Neurovascular status should be recorded pre and post procedure. If neurovascular status is still concerning post reduction and splintage, escalation and reach-back to a vascular surgeon should be considered depending on the permissiveness of the environment. If the patient had perfusion prior to a reduction and has lost perfusion post reduction, the splint should be removed and the limb reassessed. If there is still a loss of perfusion, the senior surgical decision makers must decide between angiography (if available) or immediate surgical exploration. In most cases, immediate surgical exploration will be the preferrable option unless there is significant uncertainty about the location of the vascular injury (e.g. in patients with more than one wound on a limb and no localising signs). Adequate analgesia or sedation needs to be considered to facilitate a good reduction.
Infection Control and wound management
Wounds should be assessed and consideration of damage to underlying structures assessed. Gross contamination should be removed, appropriate antibiotics administered, tetanus risk and immunisation status considered. Wounds can be covered with saline soaked gauze or non-adhesive dressings. Wool and crepe can be utilised for compression for transport.
In the event of an open fracture, refer to the Open Fracture CGO (LINK).
Open Fracture Antibiotic Recommendations – Refer to the deployed antimicrobial guidelines however, if these are unavailable, use the following as a guide:
Co-amoxiclav
1-2 months 30mg/kg every 12 hrs
>2 months 30mg/kg every 8 hours (max 1.2g single dose)
OR If Penicillin Allergic:
Clindamycin
3-6mg/kg every 6 hours (max 450mg per dose)
Early reach-back or engaging with host medical facilities to both Paediatric, Plastics or Vascular clinicians if required is essential in ensuring good outcomes for patients with complex injuries.
Non-Surgical Management of Fractures
Many closed paediatric fractures can be managed without surgical intervention. Ideally, appropriate imaging (usually radiographs) of the affected limb should be obtained to plan treatment. If imaging is not available but there is clear deformity then it is reasonable to perform a manipulation to attempt anatomical realignment and “social straightening” of the limb. See Page for Age (LINK) for analgesia / sedation doses. In children with vascular compromise and limb deformity, realignment and splinting are the first line treatment and will often restore perfusion, see flowchart above.
Splinting can be temporary with SAM splints and the Kendrick Extrication Device. More definitive treatment in Plaster of Paris (POP) can be used if available. Fully encircled, moulded casts should be avoided in the deployed setting because of the risk of swelling and compartment syndrome.
Surgical Management of Fractures
In high energy trauma and open injuries, damage control surgery (DCS) and surgical debridement may be required as per adult limb trauma management. Depending on the size of the child, external fixation may be appropriate to stabilise fractures in the first instance. If considering external fixation (Ex-Fix) remember most paediatric patients will be transferred to host nation medical facilities and the capability to manage/remove external fixation need to be considered. It is worth mentioning that within Role 2 surgical modules, there is limited kit availability for any more complex surgical management than DCS, debridement and Ex-Fix. Refer to the CGO “External Fixation (Ex-Fix) Configurations for Common Fractures” (LINK) for further details regarding the use of external fixators in the paediatric population.
Compartment Syndrome
Compartment syndrome in children is relatively rare but should be considered in all patients with extremity trauma. Presentation and management are as per Acute Compartment Syndrome and Fasciotomy CGO (LINK). It may be more challenging to diagnose as children may not vocalise or externalise pain in the same was as adults and may not be able to provide you with a clear history.
Closed Fractures
Closed fracture should be managed with assessment of the neurovascular status and splinting of the affected limb with repeat neurovascular assessment after. Reduction of the fracture can be attempted under appropriate sedation and analgesia by a trained practitioner. However, the resource-intensive nature of sedating a child and monitoring them afterwards should be considered.
Prolonged Casualty Care
Casualties with limb trauma should be evacuated along the appropriate evacuation chain as quickly as possible with their parent or guardian. Your medical plan should have details of local hospitals and the evacuation chain options, as well as the level of care they can support. You may have to utilise and adapt your equipment to the paediatric population.
Paediatric Considerations
This guideline is written specifically for the paediatric trauma patient population
