Objectives
The purpose of this guideline is to describe the application of external fixation (Ex-Fix) devices in the management of common fractures encountered during deployed surgical care. These devices are used to achieve skeletal stabilisation, particularly in resource-constrained settings.
Scope
This guideline is targeted for use across all echelons of deployed surgical care.
Audience
The audience for this document is deployed surgical team and medical support staff.
Initial Assessment & Management
Initial Assessment and Management
Injury Identification
Perform a systematic assessment to identify fractures, ensuring imaging (portable X-ray) when available. Document wound contamination, neurovascular status, and compartment syndrome signs (As per CGO Acute Compartment Syndrome and Fasciotomy). Open fracture management performed as per Wound Excision CGO concurrent to the following principles.
Principles of Fracture Management
Splint and immobilise fractures. This aids analgesia requirements and protects the soft tissue envelope associated with a traumatic injury. Assess whether the fracture needs to be reduced; and whether this can be achieved with non-invasive indirect methods such as casting, splintage or bracing. If fracture reduction is required and is not able to be held by non-invasive means, or the nature of associated injuries mandates skeletal stabilisation then consider the application of an External Fixator device.
General Principles of External Fixation
External fixation aims to achieve skeletal stabilisation through an external scaffold composed of pins and bars. This technique can serve as either temporary or definitive management. The advantages of external fixation in severe injury are due to the minimal soft tissue insult associated with the application. This enables vascular assessment and management, as well as wound debridement. The application can be expeditious, causing minimal interference with the wider resuscitation process and does not rely on radiography. Once stabilisation is achieved it optimises ongoing neurovascular assessment, patient handling, pain, and wound care. Vigilance is required to prevent complications, particularly pin site infection. Other complications include neurovascular injury, implant loosening, osteomyelitis and mechanical failure. Regular review and diligent application techniques are required to reduce this risk.
Pin Selection: The diameter of the pin size confers increased mechanical stability. A pin size should be between 1/4 and 1/3 of the diameter of the bone. Greater than 1/3 width risks fracture. Pin sizes will vary with anatomical location; see typical pin sizes below:
- Metatarsal – 3 mm (use of the 3/5 mm Hybrid Half Pin)
- Calcaneus – (5 mm Transfixing pin; also known as Denham pin)
- Tibia – 5 mm Half Pin
- Femur – 5 mm Half Pin
- Pelvis – 5 mm Half Pin
- Humerus – 5 mm Half Pin proximally, 3 mm (3/5 mm Hybrid Half Pin) distally
- Radius/Ulna – 3 mm (use of the 3/5 mm Hybrid Half Pin)
- Metacarpal – 3 mm (use of the 3/5 mm Hybrid Half Pin)
The use of Hybrid 3/5 pins in the Hoffman 3 system allows a smaller cortical diameter to be used with a connection element of a larger diameter. These are represented with numerical/numerical description with the former representing the diameter of the threaded portion of the half pin and the latter the diameter of the non-threaded shank portion for application to a connector.
Pin placement: Safe corridors of anatomic locations for pins are demonstrated within injury-specific configurations below. Principles of pin placement are: avoidance of neurovascular bundles, avoidance of tethering muscle, interference of contralateral limb or areas subjected to pressure, ability to nurse the patient in supine/seated position, avoidance of heavily contaminated wounds; maintenance of vascular access (of particular importance in polytrauma casualties).
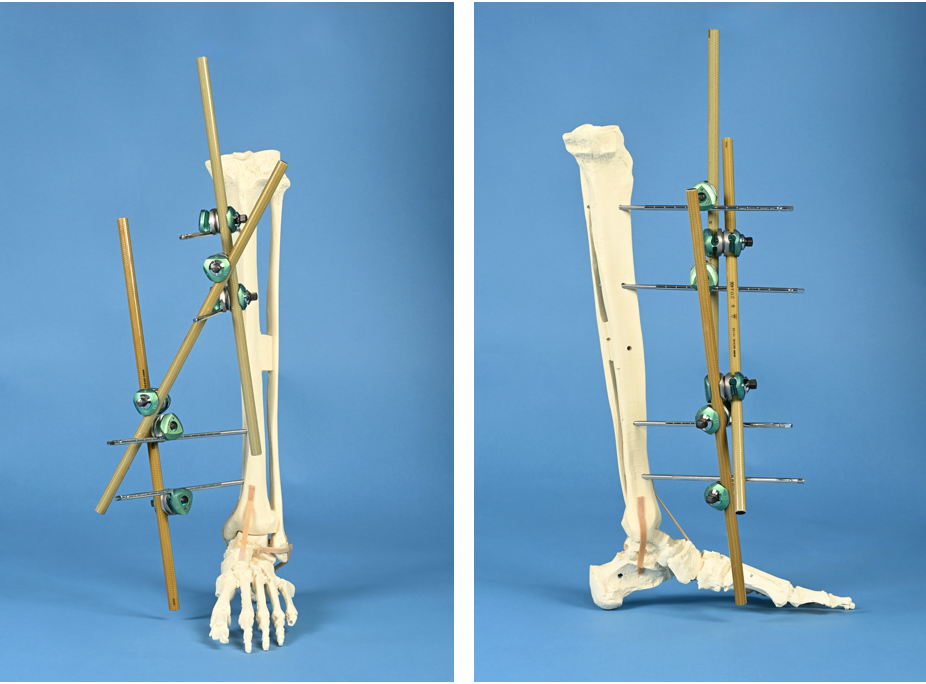
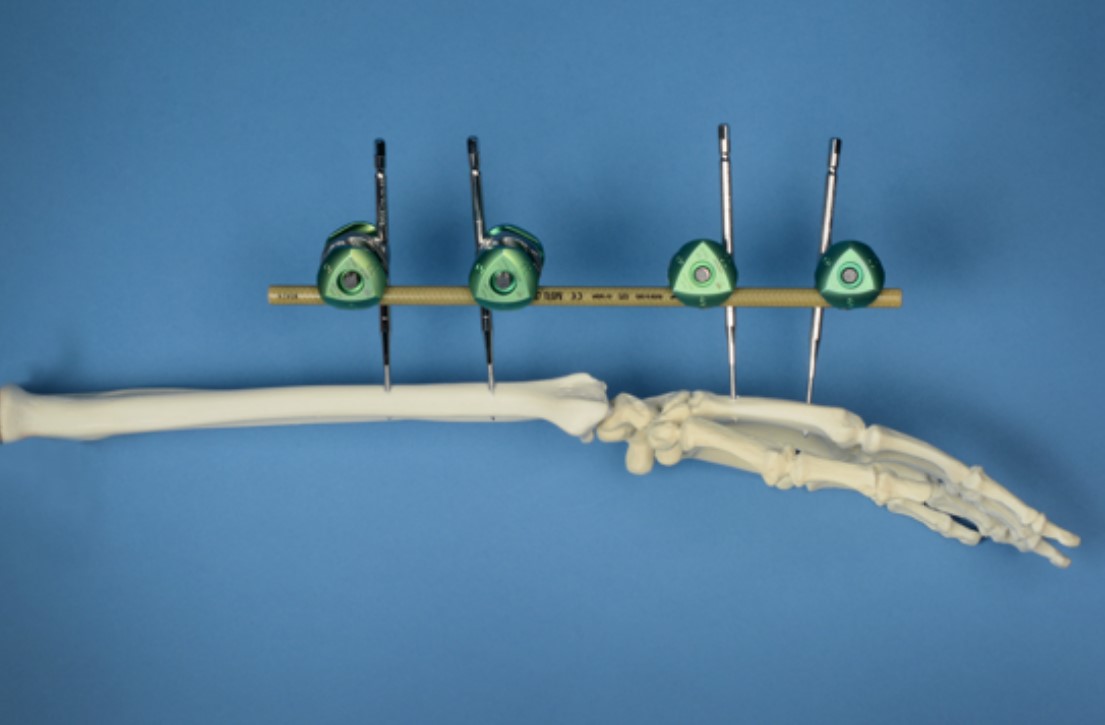
Frame Assembly: Principles of near-far pin placement (2 pins per fragment placed 1 close to fracture and 1 far from fracture) to obtain fragment stability. Consideration of avoidance of zone of injury and preservation of future operative tissue being invaded is beneficial. Ensure a minimal gap of approximately 2 cm exists between the connecting bars and the soft tissue to allow room for ongoing swelling.
Stability Considerations: Construct stability is aided by increased diameter of pins, increased number of pins, increased diameter of bars, increased number of bars, multiplanar constructs, and reduction of distance between bone and bar. Ultimately, construct stability within the context of a fracture is most stable with a successful reduction.
Componentry
The Hoffmann 3 External Fixation hardware is coordinated into three different packs/trays with individual supplementary packed items as required. From the perspective of the deployed role, these are available in two main forms: Field Kit B and the Hoffmann External Fixation System.
Field Kit B was specifically designed with the intention to deliver a forward deployed surgical pack. The formal title is “Field Kit B Hoffmann 3 Augmentation Kit”. For most of the injury patterns described in this guideline, management is presented with the aim of using minimal equipment, ideally relying on a single field pack (Field Kit B) whenever possible. The Field Kit B componentry importantly does not include Hybrid 3/5mm Apex Half Pins (for use in the upper limbs or metatarsals). At present, these must be packed and sterilised separately so may not be available in every deployed environment. The transfixation (Denham) pin is available as an individual pre-packaged and sterilised component. See below under “Supplementary Componentry”.
The Hoffmann External Fixation System is a full tray of interchangeable components and instrumentation to give the operator a wider choice and volume of hardware to augment the management of the injury. The availability of these components allows greater flexibility and tailoring of fixation to enhance stability and soft tissue protection.
Field Kit B (NSN 6516-01-627-9042)
|
Reference
|
NSN
|
Description
|
Quantity
|
|
4922-1-010
|
6515-01-600-4116
|
Delta Rod-to-Rod Coupling 5/8/11 mm Rods and 5 mm Pins
|
6
|
|
4922-8-400
|
6515-01-600-3377
|
Vectran coated Connecting Rod Ø11 x 400mm
|
3
|
|
4922-8-400
|
6515-01-513-1261
|
Apex Pin Ø5mm, 180 x 50mm, self-drilling
|
4
|
|
VIM-0
|
6515-01-208-5966
|
Drill Brace for Apex Pins and Couplings / Clamps
|
1
|
|
SW A-S10
|
NA
|
No.10 Scalpel
|
1
|
|
32-01241
|
NA
|
Mosquito Hemostat Clamp
|
1
|
Hoffmann 3 External Fixation System Tray
|
Reference
|
NSN
|
Description
|
Quantity
|
|
4922-9-950
|
6530-01-621-1211
|
Level 3/4/5 Military Plastic Tray
|
1
|
|
4922-1-015
|
6515-01-604-7102
|
Multiplanar Rod to rod-to-rod coupling
|
4
|
|
4920-9-020
|
6515-01-522-4925
|
Thumbwheel
|
2
|
|
5026-1-150
|
6515-01-600-4144
|
4 mm x 150 mm, 40 mm THD SD/ST Apex Half Pins
|
12
|
|
5026-8-120
|
6515-01-600-4135
|
Hybrid 3/5 mm Hoffmann Apex Pin
|
25
|
|
5018-6-180
|
6515-01-513-1261
|
5 mm x 180 mm, 50 mm Apex Half Pins
|
26
|
|
5018-5-150
|
6515-01-503-9984
|
5 mm x 150 mm, 40 mm Apex Half Pins
|
10
|
|
5050-4-300
|
6515-01-604-0767
|
5 mm x 300 mm, 40 mm Central thread
|
2
|
|
4922-1-010
|
6515-01-600-4116
|
Delta Rod-to-Rod Coupling 5/8/11 mm Rods and 5 mm Pins
|
16
|
|
4922-9-140
|
6515-01-600-3334
|
Soft tissue protector
|
2
|
|
4922-9-240
|
6515-01-600-3365
|
Trocar
|
2
|
|
4922-7-220
|
6515-01-600-3370
|
Semi-circular rod 11 mm x 400 mm
|
2
|
|
4920-9-036
|
6515-01-208-5963
|
7 mm Spanner Wrench
|
1
|
|
5057-0-300
|
6515-01-208-5966
|
Apex Drill Brace 3/4/5/6MM
|
1
|
|
4922-9-050
|
6515-01-600-3340
|
AO/Jacobs Quick Release Apex 4/5/6 mm Chuck
|
1
|
|
5028-8-400
|
6515-01-567-4036
|
MRI Safe Connecting Rod 8x400mm
|
4
|
|
5028-8-300
|
6515-01-567-4047
|
MRI Safe Connecting Rod 8x300mm
|
2
|
|
4920-9-030
|
6515-01-583-5135
|
7 mm T-wrench 4/5/6 mm Pin Driver
|
1
|
|
4922-8-300
|
6515-01-600-3362
|
Carbon Connecting Rod 11 mm x 300 mm
|
2
|
|
4922-8-400
|
6515-01-600-3377
|
Carbon Connecting Rod 11 mm x 400 mm
|
4
|
Supplementary Componentry
|
Reference
|
NSN
|
Description
|
Quantity
|
|
5018-6-180
|
6515-01-600-4135
|
Hybrid Apex Pin Ø3/5mm, 120 x 20mm, self-drilling
|
-
|
|
5050-4-300
|
6515-01-604-0767
|
5 mm x 300 mm, 40 mm Central thread
|
-
|
Infection
Antibiotic prophylaxis should be administered within 1 hour prior to knife-to-skin. Ongoing antibiotic prescription is not a pre-requisite of external fixator application but is related to the overall injury profile. The importance of soft tissue protection is vital for infection prevention. Skin tenting at pin sites should be prevented.
Post-Operative Principles
Reassess neurovascular status post-application. Simple elevation of the limb aids post-operative swelling and pain. Reassessment of construct stability is required at regular intervals. Patient positioning and pressure areas related to the frame must be checked. Joint mobilisation proximal and distal to the frame may be achieved to prevent contracture and discomfort. Always consider the pressure effect that the frame itself could have on other body sites such as the contralateral limb.
Wound Care
Simple wound dressings are applied to the external fixator pin sites after application. This is composed of an antiseptic-soaked swab at the base of the pin site. Ongoing pin site care is described in the prolonged field care section.
Advanced Assessment & Management
External Fixator Surgical Guidelines
These surgical guidelines are designed to act as a handrail for a standardised approach to the configuration of an External Fixator. Individual injury profiles will dictate the exact configuration of the construct. Apply the general principles of external fixation to complex injuries to allow skeletal stabilisation, protection of soft tissues and multi-speciality management.
The individual configurations have been described to use minimal equipment, primarily relying on a single Hoffman 3 Field Kit B pack when possible.
General Surgical Considerations for Usage of Hoffman 3 External Fixator
Apex Half Pins: Apex half pins are self-drilling and self-tapping; no predrilling is required. Insert perpendicular to the bone and centrally through its cross-section. Bicortical purchase should be attained for optimal stability (excluding the placement of pelvic pins). Pins are inserted manually using a drill brace with soft tissue protection. Constant steady pressure with clockwise rotation of the brace facilitates advancement. A reduction in resistance will be palpable after the first cortex. The next increase of resistance will represent the far cortex; advancement of up to 6 complete revolutions of the drill brace enable full bicortical purchase. Ensure that the skin and muscle are not tented on the half pin as this raises the chance of associated infection. Hybrid half pins are inserted in the same manner, the brace is interchangeable.
In extremis, the brace itself can be used as an ex-fix bar because it has the same diameter at the ex-fix bars and it does fit into the connectors. This statement is not a recommendation for this, but the deployed surgeon may find this information useful in resource-constrained settings.
Transfixing Pin: The 300 mm transfixing pin (Denham pin) features a 6mm threaded portion in the centre of the shank. Unlike the apex pins, it is advanced fully through the far cortex and until the threaded portion achieves bicortical engagement. The tip of the pin to requires a skin incision at the far side to accommodate it passage. To reduce the risk of iatrogenic injury a bung or protective cap may be applied to the exposed end of the pin.
Connectors: The Hoffmann kit uses Delta Couplings to link rods and pins via a ‘snap-to-fit’ mechanism. Rod-to-rod couplings (green/green) accommodate 8 and 11mm rods to 5mm pins. Rod-to-pin couplings (grey/green) support 4, 5, and 6-mm apex pins. All couplings feature a preassembled thumbwheel for provisional tightening, which may be snapped off and replaced, or once removed definitively tightened with the drill brace (which doubles as a wrench). For best fit, a coupling may serve as a drill guide when provisionally placed on a rod during insertion of the second pin.
Rods: The system uses Vectran-coated carbon fibre rods (also known as bars). Field Kit B includes three 11×400 mm rods. The External Fixation System includes additional length and diameters of rods as detailed in the componentry section.
See Below for Configurations for Specific Anatomical Areas
Prolonged Casualty Care
Stabilisation: Ensure frame integrity and reassess alignment regularly. Daily check of connector tightness. If concerns, additional stability can be achieved as per the general principles section.
Infection Prevention: A high degree of vigilance is required for pin site care; the pin sites should be checked daily. The spectrum of pin site issues can range from irritation to deep infection. If infection is suspected, then prompt administration of antibiotics is indicated with clinical reassessment.
Pin site Cleaning: This should occur weekly in the form of an antiseptic solution such as alcoholic chlorhexidine. Simple dressings can be reapplied as required. These dressings should be non-shedding. A compression clip to press the dressing against the skin can aid patient discomfort; a clip, bung or bandage can be used. Care must be taken not to push the clip and dressings down onto the skin too hard or else tissue necrosis can result. Once pin sites have become dry there is no requirement to apply any superficial dressings. However, in the deployed setting, dressings are recommended due to the austere environment and challenges with environmental cleanliness. The frequency of pin site cleaning may require to be increased in the presence of infection. Bathing is contraindicated. Showers are tolerated on the day of pin site care prior to dressing change; after showering the pin sites are carefully dried and new dressings applied. Pin sites that become painful, swollen, and discharging may be treated with oral antibiotics according to the Deployed Antimicrobial Guidelines. In severe cases of pinsite infection, the affected pin may have to be removed and re-sited.
Movement: Encouragement of proximal and distal movement of limbs once stabilised with external fixators prevent contractures. Regular positional change of patients to prevent pressure areas is critical.
Swelling: The severity of swelling can increase with time duration from injury; check that skin clearance to bars and connectors remains adequate. Simple elevation aids the improvement of soft tissue swelling. Always consider the risk of compartment syndrome.
Construct adjuncts: Consider construct of construct adjuncts such as a kickstand to allow the affected limb to be suspended; encouraging complete assessment of the affected limb. Take care to ensure constructs do not cause iatrogenic injury to the other limb or body regions via pressure.
Paediatric Considerations
Anatomical Considerations
- Use smaller pins for paediatric anatomy; apply general principles in consideration of pin diameter selection. Aim for pin diameter >1/4 but <1/3 of cortical-cortical width
- Avoid the physis when placing pins to prevent the risk of growth disturbance. In consideration of this, a minimum distance of 2 cm is recommended to prevent the risk of damage.
Monitoring and Adjustments
- Reassess frequently to address potential complications such as pin-site infection or construct loosening, which may occur more rapidly in children.
Definitive Fixation
- Due to the decreased duration of bone healing in a paediatric patient consider whether the external fixator may be used as a definitive device.